Most of us nurses got into this line of work because we want to help people. We want to help them feel better, heal from diseases and injuries, and do our best to make what’s often one of the worst experiences of their lives (being in a hospital) a little more bearable. I think this is why many of us struggle with starting IVs and venipuncture in general. Putting needles into those people we are here to help goes against our instincts and can be a very difficult thing to do, even though logically we know it’s helping them in the long run.
This kind of fear comes from a good place of course, but is detrimental to the care of our patients. When we’re afraid to insert an IV or draw blood, we will often cause more pain and harm in the process. Yes, I know those of you who are already anxious about this are saying something like “Well yeah, but calling us out like this is making it even worse!” I get it, and don’t worry, I’m here to help, read on for some solutions to this conundrum.
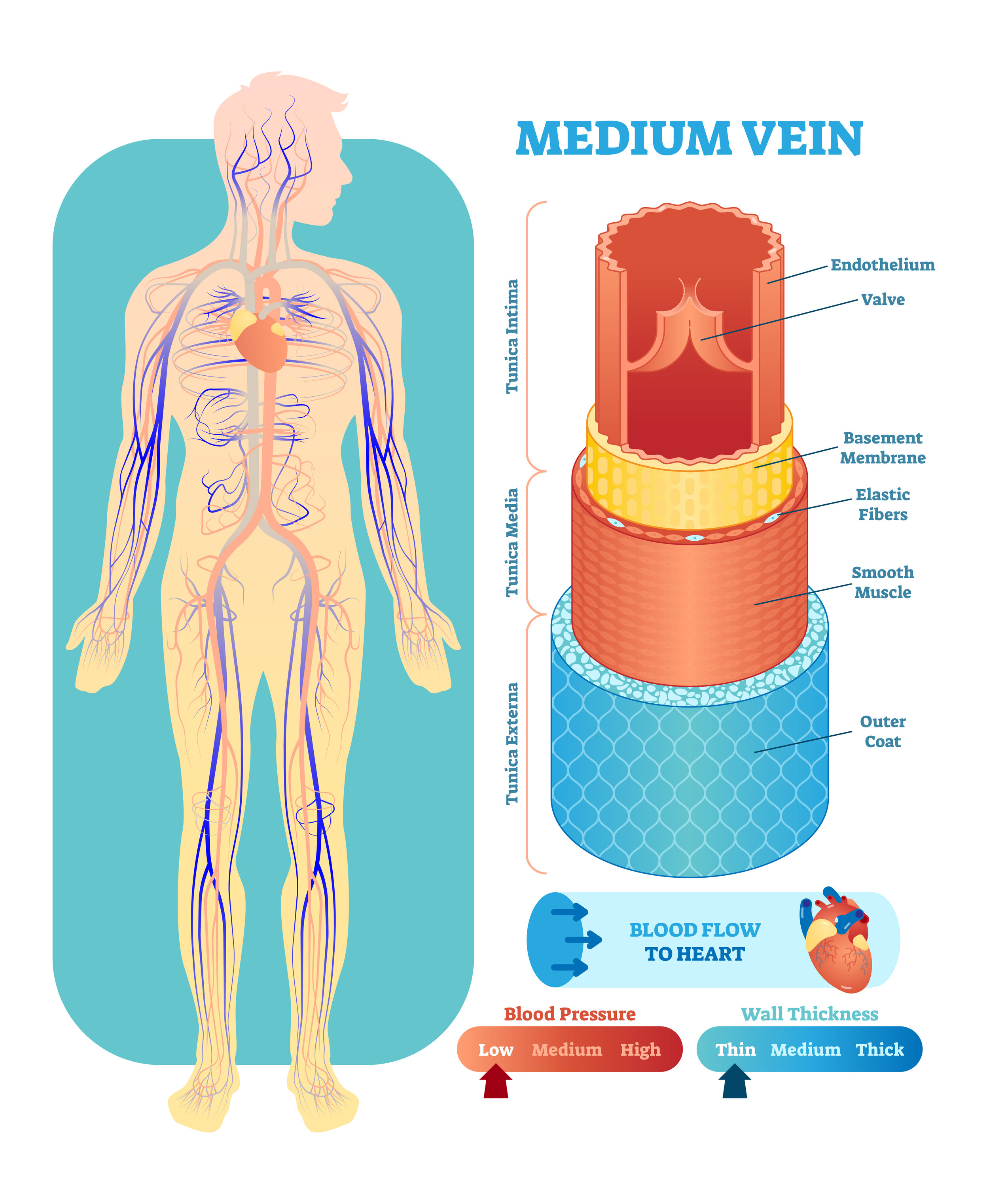
I’ve said this before, and I’ll continue to say it over and over again. The basis of good, skillful venipuncture is a proper understanding of procedures, best practices, anatomy, and policy. When you have a thorough understanding of exactly how to perform venipuncture, how to start an IV, draw blood, etc., you will automatically be less anxious than if you didn’t have this understanding. No, it doesn’t completely take away the fear of inserting a needle into someone, but it’s a necessary first step. My Instagram page and this blog are both great places to start for free information in small, bite sized bits that are easy to understand. If you want a thorough education, I have video courses specifically designed to teach you these skills in the most efficient way possible. I did my best to make them affordable by getting them approved for continuing education, which often makes them eligible for reimbursement from your employer, which should make them free. Click HERE to check out all my full-length video courses.
The next step is becoming familiar with your equipment and knowing exactly how it works, and practicing on a non-living being. I wrote an entire article about how to practice venipuncture HERE, check it out! Once you’re comfortable with the equipment you’ll be using, and there are no surprises like how does the safety work, how do I hook up the extension tubing, how do I flush the line, etc., you’re half way to becoming a confident, professional IV starter.
Causing pain is probably the biggest fear we all have. It’s the opposite of what we want to do for our patients. This one aspect can keep nurses scared for years, and prevent them from providing the best care they can. Please, PLEASE, read my ARTICLE ON PAIN MANAGEMENT and watch the video. If you’re following these methods, you’ll be reducing the pain associated with venipuncture by at least 50%-90%.
Now that you know how to perform venipuncture and how to reduce pain, but you’re still having debilitating anxiety, you’ll need to learn some calming techniques. My very favorite way of reducing anxiety is called the Physiological Sigh. Dr. Andrew Huberman has a great video about it HERE, please watch it. The basis of the technique is a swift inhale through the nose until your lungs feel full, a slight pause, then another small inhale even further through the nose, followed by a slow exhale through the mouth. 3-6 of these in a row will take almost anyone from a state of high anxiety back down to baseline. And yes, there’s plenty of science behind this, including human studies (like all the information I provide here). If you still need to calm down, or to maintain this newly achieved baseline, humming has been shown to prevent or lower anxiety as well. Sure, it might be a bit awkward to start humming around your patients, but if you pick a tune most people know, you can have your patient join in and they’ll be less anxious with you! Try to make it a little fun 😊
After this it’s all a matter of practice. Start offering to start all the IVs on your unit, watch other nurses to see how they do it, and really build your skills. With a bit of success, much of your anxiety will disappear.
That’s it for now, I really hope this helps some of you overcome your fears. If anyone has questions or suggestions, feel free to comment below, or send me an email or message on social media. Good luck everyone!